Xiao Meng is a child diagnosed with neurogenic bladder. Shortly after birth, she underwent surgery for myelomeningocele in the sacrococcygeal region. Not long post-operation, she developed symptoms including difficult urination (voiding dysfunction), recurrent fever, and urinary tract infections (UTIs). The chronic nature of her condition took its toll; by six months old, Xiao Meng appeared significantly thinner and weaker than her peers.
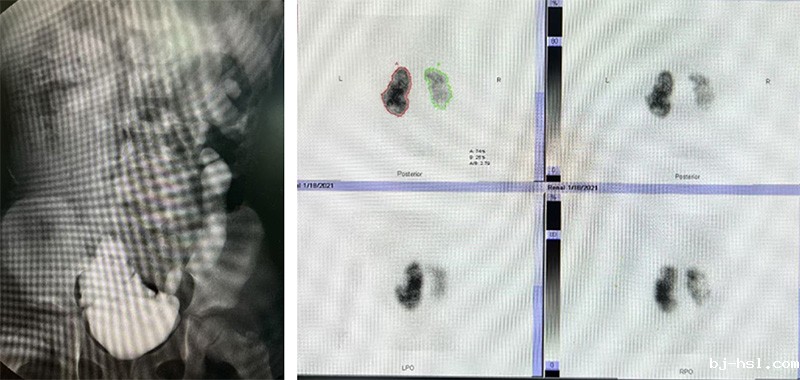
Upon evaluation at the Department of Urology, Children's Hospital of Fudan University, her bladder was identified as a "high-risk" neurogenic bladder. This diagnosis indicated not only severe bladder dysfunction, but also secondary vesicoureteral reflux (VUR), and renal impairment resulting from the recurrent UTIs.
For infants and young children like Xiao Meng, the team performed a vesicostomy. This is an interim management procedure where a small opening (stoma) is created in the lower abdominal wall. The bladder mucosa is sutured to the abdominal skin, allowing continuous urinary drainage from the bladder directly through the stoma, which can be managed using a diaper.
Post-vesicostomy, Xiao Meng's UTIs were quickly controlled, and her growth rapidly caught up with her peers. However, this was not a long-term solution. As Xiao Meng approached school age, her parents grew anxious: Could she manage the stoma care and diaper changes at school? Would constant diaper use lead to teasing or isolation?
Thanks to the decompression provided by the vesicostomy, follow-up assessments at age 6 showed significant downgrading of her bilateral VUR and no progression of renal impairment, though her bladder capacity remained largely unchanged. The surgical team decided to perform an augmentation cystoplasty (bladder augmentation) combined with a Mitrofanoff procedure. This aimed to increase her bladder capacity and create a continent catheterizable channel using the appendix, facilitating future clean intermittent catheterization (CIC). After a challenging 4-hour surgery, the procedure was successful.
Within three months post-operation, Xiao Meng adapted well. She successfully discontinued diaper use, remained free of UTIs, and no longer required prophylactic oral antibiotics. Her augmented bladder achieved a functional capacity exceeding 300ml, allowing her to stay dry with only 4-5 catheterizations per day, mimicking near-normal volitional voiding function.
Crucially, Xiao Meng's daily life and schooling became indistinguishable from other children. She attends school normally, plays happily, and makes friends.
Long-term Commitment
For decades, the Urology Department at Children's Hospital of Fudan University has been dedicated to the treatment and long-term follow-up of children with neurogenic bladder. The team provides comprehensive, life-cycle medical support and compassionate care, empowering these children and their families to overcome challenges, regain confidence, reintegrate into life, and ultimately, build a brighter future for children with neurogenic bladder.
________________________________________
Disease Overview: Neurogenic Bladder
Neurogenic bladder (officially neurogenic bladder urethral dysfunction) refers to a spectrum of disorders characterized by dysfunction of the bladder and/or urethra (specifically storage and/or voiding dysfunction) due to neurological lesions or diseases. This dysfunction leads to a range of lower urinary tract symptoms (LUTS) and complications.
The clinical manifestations of neurogenic bladder are diverse. Common presentations include dribbling, weak urinary stream, or straining during urination. If unmanaged, this can lead to vesicoureteral reflux (VUR) or obstruction at the ureterovesical junction (UVJ). Critically, it often causes febrile urinary tract infections (fUTIs), ultimately resulting in irreversible renal damage. In severe cases, it can progress to uremia, necessitating renal replacement therapy (RRT) such as dialysis or transplantation.